en.wikipedia.org/wiki/3%CE%B1-H … ydrogenase
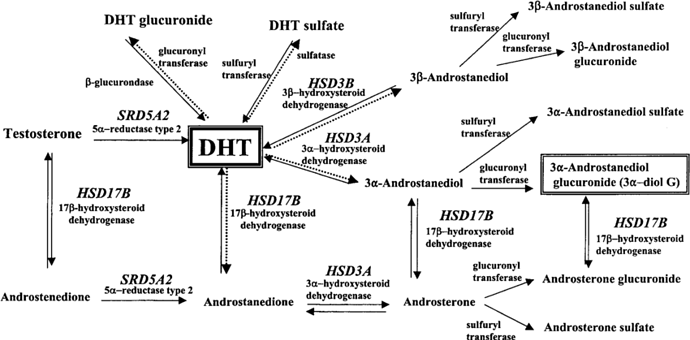
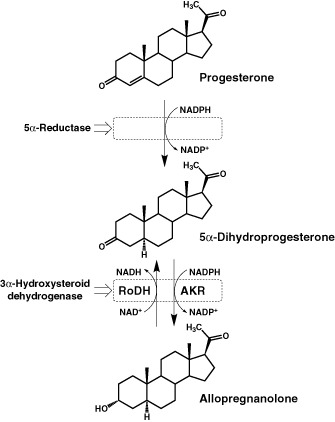
This enzyme is responsible for the conversion of both DHT into 3a-diol-g AND the conversion of a progesterone-derived intermediate into allopregnanalone. Suppression of both of these metabolites has a large effect on the GABA system, and seeing as how both are responsible for anxiolytic and pro-sexual activity, its suppression to me is by far the number one most suspicious cause of Post-Finasteride Syndrome.
en.wikipedia.org/wiki/Allopregnanolone
I think our primary goal as PFS sufferers, at least before we figure out how to upregulate 3a-hydroxysteroid dehydrogenase, should be to replace both allopregnanalone and 3a-diol-g within our systems. I understand an allopregnanalone patch or pill is currently under development for MS, and I’ve also heard that low doses of Prozac can stimulate allopregnanalone upregulation (anyone have any personal experience with this?). There was also a drug in development 5-10 years ago that would function as an analog to 3a-diol-g.
en.wikipedia.org/wiki/Ethynylandrostanediol
So many PFS sufferers exhibit consistently low levels of this metabolite.
en.wikipedia.org/wiki/3%CE%B1-Androstanediol
It seems to me that finasteride didn’t completely fuck up our 5a-reductase-2 enzymes, but screwed up the metabolism of DHT and progesterone downstream from this step. This is evidenced by most men with this condition having normal DHT and T levels, albeit maybe somewhat altered from pre-fin use, yet consistently abnormal levels of 3a-diol. Some men even report improvement with progesterone cream, perhaps because it has an affect on upregulating this enzyme, or at the very least an increase in progesterone will theoretically cause a proprtional increase in allopregnanalone, despite a decrease in 3a hydroxysteroid dehydrogenase activity.
pfsfoundation.org/published-research/
It’s not even completely understood whether the pro-sexual effects men feel are from DHT metabolites or T/DHT themselves. So it may very well be that high T and DHT only induce androgenic effects when they’re converted into their end metabolites, which may be 3a-diol-g, or compounds even further down the line.
The analog of 3a-diol-g was apparently discontinued, but it and perhaps other analogs are, to me, the most important things to look into right now. I look forward to what the Baylor study comes up with, and hopefully it will corroborate what seems to me to be self-evident at this point. Until the results are published, I think we should speak to MD’s that recognize PFS and discuss this possibility with them. If the metabolism of DHT into 3a-diol-g is truly the main problem that we face, then (hopefully) the treatment could be as simple as replacing the deficient 3a-diol-g and restarting the androgenic metabolic pathway.
At this point, looking at all of the published research and lab results of PFS sufferers, I have almost no doubt that finasteride use downregulated 3a-hydroxysteroid, and the sudden surge of DHT following its discontinuation overwhelmed these enzymes and perhaps derailed their ability to convert DHT and progesterone into 3a-diol-g and allopregnanalone, respectively, among potentially other metabolic conversions they’re responsible for.
A little about myself. I took finasteride for only 8 days (fuck me, right?), and 4 days upon withdrawal, I crashed with severe symptoms. I’ve improved a bit since then, but I’ve never really been completely back to normal, like most of you. This happened in early September 2016. I’ve been lurking on this site and searching for answers ever since. I’ve tried Ashwagandha, Vitamin D, Tyrosine, 5-HTP, probiotics, heavy weightlifting, cardio, fish/flaxseed oil, tryptophan, melatonin, turmeric, cannabidiol, zinc, iron, etc. all with marginal results. I recently started an intense probiotic regimen consisting of VSL 3 and Prescription Assist probiotics, as well as a ketogenic diet. Now that I’ve learned as much as I have, I doubt this will affect my illness, but at the very least it should hopefully do something about the IBS and acid reflux I have. The only real hope I have with this protocol for PFS is if it somehow reduces inflammation in my body far enough that my endocrine system can focus on correcting its 3a-hydroxysteroid issue, but that’s a huge stretch.
Still, I’m happy I’ve finally figured out what’s wrong with me (with more confidence than any other idea, anyway). I’ll do my best to address this theory with medical professionals well versed with PFS (thank you for providing me with their names). I encourage you all to do the same. At this point no other theory makes as much sense as this. The Androgen Insensitivity theory was the last one I ran with, but then so many of you have attempted supraphysiologic levels of Testosterone with no improvement in your symptoms whatsoever. There are studies showing that very, very high T levels will mitigate Partial Androgen Insensitivity, but this seems to not be the case with PFS, so that’s out. The 5-ar-2 dysfunction theory is sort of the go-to theory, and it made sense to me until I began losing my hair again, just as much as I had been losing it before (Finasteride turned out to be completely fucking pointless). So my 5-ar-2 enzymes seem to be functioning at least close to properly. The gut microbiome theory is a huge stretch, but before I came across the significance of 3a-hydroxysteroid dehydrogenase it was the last thing I had left. I’ll let you all know about my personal results with this regiment at the end of August (BrongFogBoy did it for 2 weeks, I’ll be doing it for 4 weeks just to cover all of my bases).
Let me know what you all think.