how was your cognitive function/brain fog… did it go away?
In a situation where immunity is dominant, what is the response of your pelvic muscles to this? Does your bowel movements cause shrinkage? Is there an increase in intensity of the response contractions of the pelvic area while standing but not sitting and lying down?
My side effects are constantly fluctuating during the day, My Ed before bed problems are reduced by 80%, When I wake up and in the mid-afternoon like shit, It usually gets worse after eating. I can feel your pelvic muscles tightening. Could this be related to immune dominance?
I’m on anti TNF for rheumataiid
This is one of the primary symptoms that was cured for me and I can affirm it was 100% gut related in my case. I had very high D-lactate level that causes a phenomenon so called lactic acidosis. Read on it.
So, by hijacking my diet plus taking probiotics known to help reduce d-lacate levels I saw improvement in brainfog. I remember suffering extreme muscle soreness after every workout! I don’t get it anymore. I work full-time now and feel I can tackle complicated tasks better than previous years.
it works?
No change to PFS unfortunately. When I floated inflammation to my rheum Proff he said the anti TNF was the best thing around.
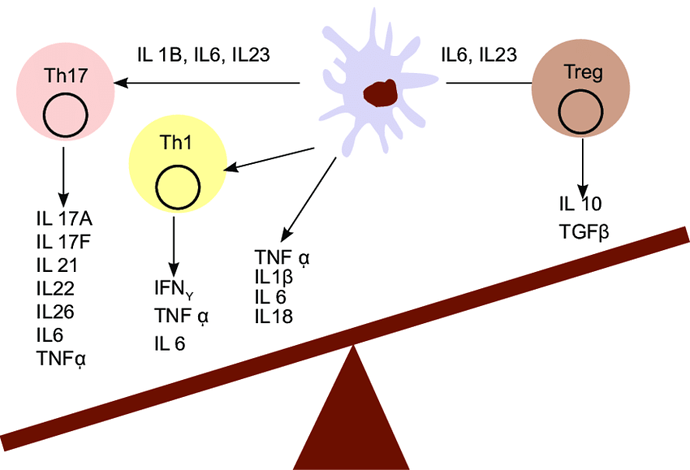
Immune system over-activation may cause increased inflammation in all body tissues including muscles, joints, brain, skin, nerves, etc. At some point, I had extreme lower back/pelvic muscles pain before and after bowel movements. Having a sedentary job was painful, literally. Moreover, walking for more than 20-30mins would gave very sore/inflammed pelvic muscles that sometimes took days to calm down.
Adrenals defends the body against inflammation. They work overtime to releasing stress hormones to lower it to make pain tolerable. Problem is when this inflammation becomes chronic.
Yeah, and that inflammation youre talking about, does not necessarily show in serum cytokines, from what Ive read…
Read on low grade inflammation @surviveplz . My CRP was well within normal range when I had my worst inflammation attack.
Yeah… im trying to fix this… Im currently on carnivore, injecting 10mg Thymalin/day, chamomille tea, garlic, magnesium, etc…
If you are going to try FMT consider which clinic you choose. In a video which they were doing a scientific study with FMT they first administered laxatives plus they did multiple sessions. I do not know if every clinic does this, but at least the laxatives should be done I think to make room for new bacteria.
Could the high İge value be related to this, doomed? Alopecia areata after accident, allergic rhinitis, I have had urticaria and these are still happening actively on my body , I was also diagnosed with prostatitis
Topics have been posted about IGE on this forum and other forums. To me, it seems like ALMOST everyone tests with high IGE antibodies which I feel is very interesting
In order to lower inflammation, try and make a checklist. This is an example:
- Is Vitamin D level ok?
- Do I have any metal or foreign material implants fixed? Teeth amalgams? Titanium screws? Fillers?
- Did I have any infections? Food poisoning?
- Do I suffer IBS symptoms? Get a stool test done.
- Do I have chronic allergies?
- Check for blood parameters (CBC, liver, kidneys, CRP, food allergy test, serum ferritin, etc.)
- Too much physical or mental stress?
- History of antibiotics? NSAIDS? Other drugs?
You need to check each item 
Precisely. I’m currently researching clinics but options are still very much limited due to Covid-19/20. You’re absolutely correct that one needs to pave the way for new microbiome shift to take place. This topic is hotly debated but I’m of the opinion that shifting microbiome isn’t as easy as I originally thought. It takes months (if not years depending on baseline) and doing this without data (i.e microbiome analysis) is shooting at moving target in the dark. Fortunately, my suggested donor is a close relative who is both young and healthy and, above all, without history of antibiotics/finesteride/etc. That said, meticulous screening is an absolute must.
I’m at a much better place in terms of symptoms and recovery but the mere thought of 100% recovery is one that’s hard to resist 
What if the answer is yes to all
Congrats @LazarusRy You’ve just got yourself proper diagnosis and is now ready to embark on your first real journey to healing. You need an action plan. Start with easy-to-fix items as you tackle the harder ones gradually.
@doomed80 thanks as nothing has worked and I have 3 pages of symptoms that have only worsened with time what would be your proposed easy fix items. What were they for you and what wee the how’s? Any advice is appreciated
Things that worked in the past:
TRT + Cortisone + low dose proviron
HGH + Cortisone
I focused on hormones back then and these two were my sure ways to feel 100% recovered but are clearly lifelong. So, I stopped and went back to the drawing board to seek a more sustainable regimen. Lights went on when I accidentally took Xifaxan/Rifaximin for chronic constipation and noticed immediate improvement in grueling brainfog and other PFS-like symptoms. This is when I first learned that gut must somehow be involved. I spent next 2 years reading on gut, microbiome, immune system, and inflammation. I had my microbiome analyzed to see what abnormalities exist and then read more on diets, probiotics and prebiotics to promote gut healing, increase bacterial diversity, and encourage missing bacteria.
Problem is, this is extremely individual so in order for me to provide a good advice, I’d need more data regarding you current microbiome. Maybe try uBiome or ThryveInside for analysis? @LazarusRy