I know this post may come off a bit of topic. But I see some similarities between TBI (traumatic brain injury) / CTE (chronic traumatic encephalopathy) and PFS:
- both share symptoms like fatigue, memory impairment, sleep and mood disruption, changes in personality
- both show that the gut-brain-axis is affected (disrupted gut bacteria)
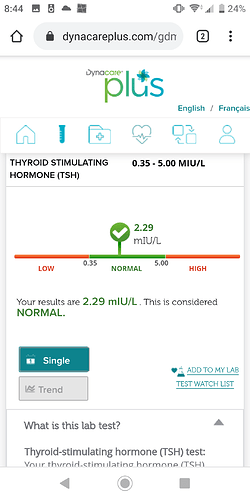
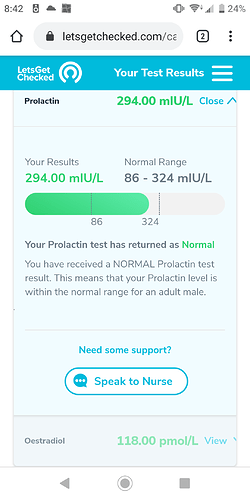
- both show disruption in hormone profiles
In this article:
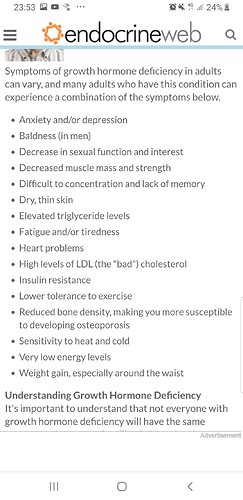
They showed that GH (growth hormone) is reduced in TBI and that it may account for fatigue etc. Also it should have a protective effect on the brain. It is responsible for muscle and tissue growth (PSF has muscle and tissue shrinkage), it protects against osteoporosis (PFS has increased osteoporosis risk). Growth hormone is mainly released during high intensity exercise (which could be the reason why some PFS patients had some success under exercise). The article also stated that hormone replacement with GH would stop the fatigue as long as it is given.
They also said the TBI patients had lowered or different amino acid values in their blood (amino acids are also raising the growth hormone. They think it is the altered gut bacteria are the reason, why the gut can’t absorb the amino acids well and that this may lead to the low growth hormone.
Now the question:
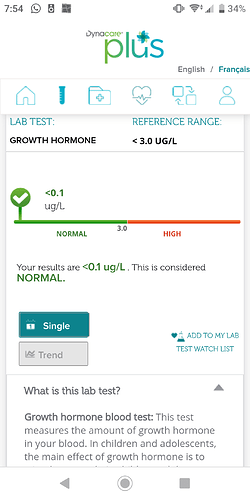
- did anyone ever look into growth hormone levels in PFS and PSSD to see if it may be low?
- as the gut microbiom is also disrupted in PFS (and maybe in PSSD), are the amino acid levels also altered and how does that affect hormone levels and muscle mass?
Has anyone heard of GH ever been tested in PFS/PSSD?