As I am looking into it I am becoming convinced our P450 enzymes are no more normal. We need to investigate it. Maybe CYP3A4 and other P450 enzymes are permanently turned off.
P450 deficiency can affect vitamin D, Testosterone, DHT etc. Almost all of the drugs or substances we have used to cause PFS are P450 inhibitors.
These have been causing PFS like symptoms and all are inhibitors of P450 mainly cytochrome P450 (CYP) 3A4
Trigonella foenum-graecum (Fenugreek) : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621675/
ketoconazole: https://pubmed.ncbi.nlm.nih.gov/21235585/
Saw Palmetto (Betasitosterol ): https://pubmed.ncbi.nlm.nih.gov/17336049/
Curcumin : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770025/
Anastrazole (Arimidex): https://pubmed.ncbi.nlm.nih.gov/9152599/
Accutane: https://www.rxlist.com/accutane-drug.htm#interactions, https://pubmed.ncbi.nlm.nih.gov/15116059/
Metformin: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3205227/; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1978432/
ciprofloxacin , Fluoroquinolone : https://pubmed.ncbi.nlm.nih.gov/8894516/
Green Tea: https://pubmed.ncbi.nlm.nih.gov/27518169/
from Wiki
[3] Symptoms of severe forms of PORD include ambiguous genitalia in males and females, congenital adrenal hyperplasia, cortisol deficiency, and Antley–Bixler skeletal malformation syndrome (ABS), while symptoms of mild forms include polycystic ovary syndrome in women and hypogonadism in men.
Are there any supplements/medication that can fix p450 enzymes?
At this stage it is a theory. We will have to go through some lab tests to find if we really are deficient in P450, if yes then which P450 enzymes?. The treatment option will come later if the theory is really proved true.
I also feel Lyme disease, Celiac disease, IBS and some other allergies are linked together through the impairment of different enzymes of P450 family.
Here you go
Characteristics of celiac disease point to impairment in many cytochrome P450 enzymes, which are involved with detoxifying environmental toxins, activating vitamin D3, catabolizing vitamin A, and maintaining bile acid production and sulfate supplies to the gut. Glyphosate is known to inhibit cytochrome P450 enzymes. Deficiencies in iron, cobalt, molybdenum, copper and other rare metals associated with celiac disease can be attributed to glyphosate’s strong ability to chelate these elements.
I had undiagnosed celiac disease with daily gluten consumption during the time I took finasteride and developed PFS.
Alex50 can you still you use Gluten ? Or yourMaybe it has now intensified.
how your celiac has changed after pfs?
I don’t know how it can be an autoimmune when so many different drugs and herbs are causing the same effects (including 5AR inhibitors and non-inhibitors). How the same antibodies can be produced from different substances? This is why after finding this I backed off from my Abodies theory. There is only one commonality, P450 inhibitors. If there is any Abodies then it might be against this enzyme P450. All the fingers are pointing at P450 enzymes, not sure if we are producing P450 less now or it is not active due to some mechanism. If it was a simple question of T or DHT then it would be a narrow problem and would have gone long ago. Our issue is broad and wide. We are deficient in other hormones as well.
Instead of speculating we should find and go for P450 testing now.
I had celiac disease diagnosed via serology and endoscopy. Celiac is a genetic condition that is typically triggered later in life. I suspect mine triggered when I developed travelers diarrhea. I still cannot eat gluten, after being strict gluten free for so long, just the tiniest amount of gluten triggers an autoimminue reaction and severe stomach pain, diarrhea, etc…
I wonder why I have been intolerant to sodium butyrate and ghee for a long time. And I think about intolerance to really small amounts (it worsens my general health, in particular gives a very strong headache and reddening of the face). So look what I found:
"Cytochrome P4501A2 (CYP1A2) activity in liver was not significantly affected in soybean oil fed rats, while it decreased on cow ghee diet by 42.1 per cent at 5 wk and thereafter did not change significantly in either group. In cow ghee group the magnitude of hepatic CYP1A2 activity was lower than in soybean oil fed rats by 47.5 and 44.2 per cent at 5 and 44 wk of dietary treatment, respectively. "
I haven’t found any other good answer to why I am responding so badly to sodium butyrate and ghee. Could it make sense? Could some of us have P450 enzymes so low that even ghee destroys us?
I have quoted this research before and it clearly show P450 can be altered by Betasitosterol.
These results suggest that decreases in plasma steroids by β‐sitosterol are possibly due to alterations in cholesterol availability to P450scc (enzyme that converts cholesterol to pregnenolone) or P450scc activity. β‐Sitosterol also appears to affect gonadal steroidogenesis between pregnenolone and Testosterone . These findings strengthen the suggestion that β‐sitosterol could be a contributing factor to the reproductive dysfunctions observed in BKME‐exposed fish.
The point here is β‐Sitosterol changed P450 activity in the affected Gold fish, so why not this can be applicable to mammals?
I think we should validate this theory through P450 lab testing to see if after using Fin/SP we have normal level of P450 enzymes in our liver and intestines. Liver and intestines are two organs where this enzyme is mainly found.
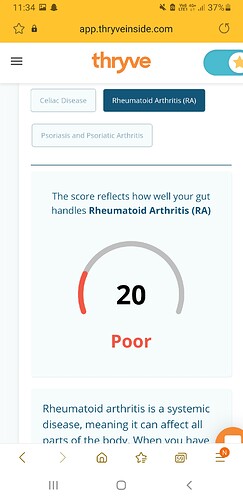
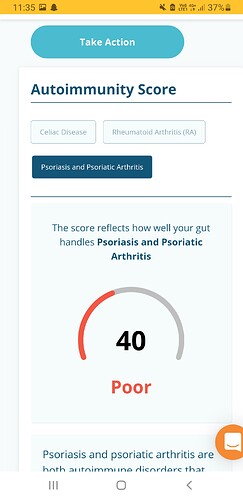
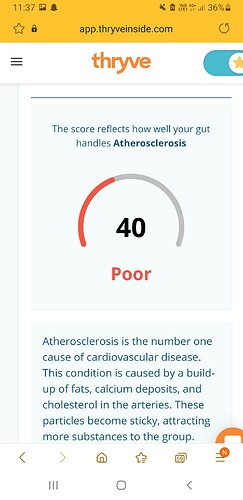
I’m just theorizing but both sodium butyrate and ghee are laden with butryic acid. While butyrate (SCFA) is good as anti-inflammatory, one can possibly have too much of a good thing. Sodium Butyrate gave me diarrhea when I ingested some 600mg/d. I read somewhere it causes reduction of butyrate producing bacteria. Reddening of face (flushing) and headache can be symptoms of increased histamine. I have a friend who had his microbiome analyzed and found out that his butyrate level is high yet his propionate (another SCFA) is very low. He displayed many symptoms of autoimmunity, which was also demonstrated in his microbiome analysis. I’m attaching some screenshots.
Screenshot_20210422-233249_Samsung Internet|243x500
There do exist Abodies against cytochrome P450 enzymes P450scc, P450c17, and P450c21
Autoantibodies to cytochrome P450 enzymes P450scc, P450c17, and P450c21 in autoimmune polyglandular disease types I and II and in isolated Addison’s disease
Thanks for your comments. I have wondered before about a possible histamine intolerance, but I am not getting consistent results. For example, if I eat 200-300 grams of cheese, sausage or salami (not a staple in my diet, but I do eat occasionally during my rare cheat days), I usually don’t get any reaction. Though I might expect them, bearing in mind that these are some of the worst products for people with histamine intolerance. I react a bit badly to sauerkraut (also troublesome for people with histamine intolerance), but only if I eat too much of it (e.g. 300 grams), but about 100 grams of sauerkraut or pickled cucumbers is already ok.
Histamine intolerance, mast cell activation syndrome, leaky gut syndrome, and small intestines bacterial overgrowth are just terms for gut-immune system dysfunction of some sort. Scientists latest belief that over 70% of the body’s immune system lies within the gut may help shed more light on the importance of having balanced microbiome. My histamine producing bacteria did not turn out high contrary to my original belief. However, I had adverse reactions to many foods. Symptoms included brain fog, tinnitus, PEM, ADHD, body aches, headaches and others. Most fellow members blame it on anti-5ar activity. I beg to disagree. These are symptoms of excess inflammation in my case.
So, I’ve been working on finding a fix through a number of approaches that include intermittent fasting, AIP diet, prebiotics, and probiotics. Results are optimistic thus far. @hrihor
Sorry if I deviate from the main topic of the thread. In such a situation, I would ask the admin to move my post (and maybe the two before) to one of the autoimmune themes.
I admit that I also have my doubts about the malfunction of 5ar (or the entire reductase mechanism) as the sole cause of our condition.
I recently wrote that I had to end AIP after 12-13 days due to a significant worsening of symptoms. On the other hand, however, I am getting promising results during my juice fast, after which my gut starts to work very well and I am beginning to tolerate a lot of problematic food products. And I think this is a solution for me and for others for whom AIP is too difficult - the use of periodic juice fasts (it is quite safe for heavily damaged organisms compared to water fasts, and maybe even better, because the body is nourished all the time, and the intestines are generally at rest as well).
I know that you are not a strong supporter of natural probiotics, but I think they can be a good solution for someone who cannot afford expensive comprehensive tests of the gut microbiome (of course, if it does not have, for example, histamine intolerance, but it affects a small part of people and additive seems easy to spot when eating sausage or cheese).
See this study: https://www.mdpi.com/2072-6643/13/5/1516/htm
For example, look at such sauerkraut (which is popular in my area - Central Europe). Basically, the immune function of cabbage leads to some homeostasis.
"Furthermore, sauerkraut is a unique source of LAB [119–121]. LAB are major species
considered as probiotics that promote innate and adaptive immunity and attenuate inflammation
through modulating gut microbiota [122,123]. For example, in a study, administration
of LAB strains to BALB / c mice attenuated allergen-induced airway inflammation
by regulating Th1 / Th2 balance and up-regulation of Tregs [123] ".
"Sauerkraut derived-LAB modulate immune function and enhance antibacterial response by inducing bacteriocins and IgA secretion [124,125]. LAB strains extracted from fermented cabbage could display immunomodulatory and anti-inflammatory activity in ovalbumin-sensitized BALB / c mice by downregulation of TLR-4 expression and modulation of B-cells and T-cells responses [126] ".