Researchers Identify Physiological Evidence of ‘Chemo Brain’
Released: November 27, 2012
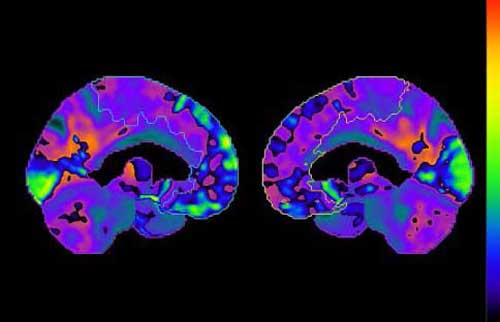
CHICAGO—Chemotherapy can induce changes in the brain that may affect concentration and memory, according to a study presented today at the annual meeting of the Radiological Society of North America (RSNA). Using positron emission tomography combined with computed tomography (PET/CT), researchers were able to detect physiological evidence of chemo brain, a common side effect in patients undergoing chemotherapy for cancer treatment.
“The chemo brain phenomenon is described as ‘mental fog’ and ‘loss of coping skills’ by patients who receive chemotherapy,” said Rachel A. Lagos, D.O., diagnostic radiology resident at the West Virginia University School of Medicine and West Virginia University Hospitals in Morgantown, W.V. “Because this is such a common patient complaint, healthcare providers have generically referred to its occurrence as ‘chemo brain’ for more than two decades.”
While the complaint may be common, the cause of chemo brain phenomenon has been difficult to pinpoint. Some prior studies using magnetic resonance imaging (MRI) have found small changes in brain volume after chemotherapy, but no definitive link has been found.
Instead of studying chemotherapy’s effect on the brain’s appearance, Dr. Lagos and colleagues set out to identify its effect on brain function. By using PET/CT, they were able to assess changes to the brain’s metabolism after chemotherapy.
“When we looked at the results, we were surprised at how obvious the changes were,” Dr. Lagos said. “Chemo brain phenomenon is more than a feeling. It is not depression. It is a change in brain function observable on PET/CT brain imaging.”
For the study, Dr. Lagos and colleagues analyzed PET/CT brain imaging results from 128 patients who had undergone chemotherapy for breast cancer. They used special software to help discern differences in brain metabolism before and after chemotherapy. Results were correlated with patient history, neurologic examinations and chemotherapy regimens.
PET/CT results demonstrated statistically significant decreases in regional brain metabolism that were closely associated with symptoms of chemo brain phenomenon.
“The study shows that there are specific areas of the brain that use less energy following chemotherapy,” Dr. Lagos said. “These brain areas are the ones known to be responsible for planning and prioritizing.”
Dr. Lagos believes that PET/CT could be used to help facilitate clinical diagnosis and allow for earlier intervention.
Research has already shown that patients with chemo brain can benefit from the assistance of nutritionists, exercise therapists, massage therapists and counselors. In one study, cancer patients receiving chemotherapy complained of losing their ability to prepare family meals.
“When the researchers provided these patients with written and planned menus for each meal, the women were able to buy the groceries, prepare the meals and enjoy them with their families,” Dr. Lagos said.
Dr. Lagos and her fellow researchers hope that future studies will lead the way to better treatment for patients experiencing this often debilitating condition.
“The next step is to establish a prospective study that begins assessing new patients at the time of cancer diagnosis,” she said. “The prospective study has the potential to establish an understanding of the change in brain neurotransmitters during chemotherapy, which may lead to improved treatment or prevention.”
Coauthors are Jame Abraham, M.D., Gary Marano, M.D., Marc Haut, Ph.D., and Sara Kurian, M.S.