Has anyone done research what effect corticosteroids have on sexual function and on other hormones such as testosterone, DHT, etc? As I wrote above, corticosteroids killed my libido (and produced depression/anhedonia/apathy) when I took them long before I had started finasteride. So at least that’s some indication that they do have an effect on androgens. Whether it is the right effect is a different question. It is entirely possible that they reduce angrogens which may in fact be beneficial for PFS. Or not.
Interesting observation @Sibelio, and the answer is yes. I’m aware of several temporary improvements with dexamethasone. You may be interested in this: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2265.2009.03683.x
Relative expression of SkM androgen receptor was similar in male (1·63 ± 0·37) vs. female (1·57 ± 0·30) subjects, despite the significant difference in plasma testosterone levels…Following dexamethasone, there was a significant down‐regulation of SkM androgen receptor (1·60 ± 0·23 vs. 1·11 ± 0·16, P < 0·05)
This is quite interesting. Do you know how temporary/permanent the improvements were? If they were just temporary, did PFS return to baseline after a period of time or did the baseline change? If so, I wonder if a longer term treatment with dexamethasone would not elicit a more permanent response as potential epigentic changes make ARs permanently downregulated. Have you considered taking dexamethasone yourself, @axolotl?
After an initial profound improvement it stopped working entirely for the person i spoke to about their experience (xptriado). And no, I don’t consider there to be a basis for expecting that as the driving factors (in terms of genomic loci/expression) are unknown. In terms of myself: No, I don’t believe it’s safe - particularly for severe cases - to mess with things with antiandrogenic properties at this stage of understanding.
Sorry don’t have much to add here. I don’t understand medically how “methyl steroids” could effect sexual dysfunction other than the term “steroids.”
I CAN report that my “sexual plumbing” continues to work fine since June 2017. Like PFS never happened.
I do encourage others to try the intravenous procedure I “endured” for five days. See my med note. It could be a total waste of time, could be helpful, who knows? I don’t think it’s dangerous, as it had no effect on me other than possibly ameliorating sexual dysfunction.

Hello, thanks for your story. I have a question about your ejaculation volume and orgasm quality: After got cured, are those symptoms are 100% back to normal (pre-fin) state too? How well they function right now? Thanks… Also you may would like to check out my story from here: 2 Sexual side effects from 2 doses of Accutane. Is there anyone like me in the world?
Thanks!!
Like I said, it’s exactly like I never experienced PFS. Everything normal. I may have even recovered to my pre-1999 state before 15 years of fin. I don’t really feel comfortable explicitly discussing details.
so, has anyone else tried an injection of methyl steroids? If not - I may bring this to a health provider to try to mimick your experience.
Interesting.
A huge dose of glucocorticoid reset you.
I used betamethasone and dexamethasone and everytime I feel better and smarter.
Andrea, I’m curious how you were prescribed the medications, and if the feelings continued to last. I believe PFS is autoimmune related, and would like to get the correct tests to confirm and be treated.
My dad is a doc.
I used to have dermatitis (now only if I use hormones) so glucocorticoids were necessary.
The effect lasts until you take it.
Correlation with immune system is sure.
Androgens and estrogens interacts with immune response.
@Andrea possiamo sperimentare una megadose di Metilprednisolone.
Io in realtà ci avevo già pensato, ma la mia endocrinologa non me lo da.
It’s interesting.
However a huge intravenous dose (1g) of methylprednisolone without any sure diagnosis could have severe side effects (also cardiac arrest).
Helpful “top notch” medical research!
Peripheral Nervous System Involved in PFS Patients with Severe ED, New Study Demonstrates
SOMERSET, N.J., April 18, 2017 – Post-finasteride syndrome (PFS) patients suffer from altered levels of critical brain-function regulators, including neuroactive steroids, according to a new clinical study published in The Journal of Steroid Biochemistry and Molecular Biology.
Titled Neuroactive Steroid Levels and Psychiatric and Andrological Features in Post-Finasteride Patients, the three-year study also uncovered evidence of neuropathy of the pudendal nerve among those with severe erectile dysfunction.
In all, 16 men with PFS and 25 control patients were evaluated in the study conducted at the University of Milano’s Department of Pharmacological and Biomolecular Sciences by a team of 12 researchers led by Roberto Cosimo Melcangi, Ph.D. The PFS patients had discontinued finasteride for a median of 5.4 years at the time of evaluation, and had no prior history of erectile dysfunction or depression prior to finasteride use.
Key findings of the study include broad effects on plasma and cerebrospinal fluid (CSF) neuroactive steroid levels observed in 14 PFS patients, as compared to 25 controls. Statistically significant decreased levels of DHT, pregnenolone, progesterone, 17-beta estradiol and dihydroprogesterone (DHP), and increased levels of DHEA, testosterone and 3-alpha diol were observed in the CSF of PFS patients.
In plasma, statistically significant decreased levels of DHP and allopregnanolone, and increased levels of pregnenolone, DHEA and testosterone were observed.
Decreased plasma levels of allopregnanolone and decreased CSF levels of progesterone are common features of anxious/depressive symptomatology. Important physiologic effects of neuroactive steroids on brain function include neuroendocrine control of reproduction and sex behavior, synaptic plasticity, morphology of neurons and astrocytes, maintenance of cytoskeleton proteins and myelin, adult neurogenesis, and cognition-related functions.
The study also identified, in 25 percent of PFS patients, the first objective evidence of abnormal somatosensory evoked potentials (SSEP) of the pudendal nerve. Abnormal SSEP findings were observed in PFS patients with severe ED.
Peripheral neuropathy of the pudendal nerve, the major nerve supplying the genitals that is critical for peripheral neurogenic control of erection, in PFS patients is a novel finding that demonstrates for the first time involvement of the peripheral nervous system in PFS patients with severe ED.
Additionally, 50 percent of the PFS patients were diagnosed with major depression based on the results from validated questionnaires, the Mini-International Neuropsychiatric Interview, the Beck Depression Inventory and the Beck Anxiety Inventory.
Such depression represents the first confirmation of findings in research led by Shalendar Bhasin, MD and published last year in The Journal of Clinical Endocrinology & Metabolism (Characteristics of Men Who Report Persistent Sexual Symptoms after Finasteride Use for Hair Loss), which suggested that men who experience persistent sexual dysfunction after discontinuing finasteride have “neurobiological abnormalities.”
“Among the most important milestones of Professor Melcangi’s research is that it builds directly on Dr. Bhasin’s work,” said Dr. John Santmann, CEO of the Post-Finasteride Syndrome Foundation, which sponsored the study.
“Medical science is now one step closer to characterizing the underlying biologic mechanisms of PFS, which in turn promises to pave the way for the development of effective therapies,” he added.
The full JSBMB study is available here.
Post-finasteride syndrome occurs in men who’ve taken finasteride to treat hair loss, or enlarged prostates. Reported symptoms include: loss of libido, erectile dysfunction, depression, suicidal ideation, anxiety, panic attacks, Peyronie’s disease, penile shrinkage, gynecomastia, muscle atrophy, cognitive impairment, insomnia, severely dry skin and tinnitus. The condition often has a life-altering impact on victims and their families, such as job loss and the breakup of marriages and romantic relationships, while also being linked to suicides.
As of April 2107, the World Health Organization Programme for International Drug Monitoring’s database of adverse drug reactions contained 13,533 finasteride ADRs, including 2,694 reports of erectile dysfunction, and 3,109 psychiatric disorders including 44 completed suicides and 31 suicide attempts.
In March 2015, the U.S. National Institutes of Health listed PFS on its Genetic and Rare Diseases Information Center, noting that “some patients who have taken finasteride have referred to side effects such as sexual dysfunction and depression (sometimes severe)… Studies sponsored by the NIH and other organizations are underway to better understand the effects of 5-alpha reductase inhibitor drugs.”
Does anyone have swollen lymph nodes?
I wonder if the 5-ar enzyme in the CNS never regenerated and that’s why we have low levels of DHT in the CNS vs. serum levels.
Well I’m not following you all. The key finding is " suffer from altered levels of critical brain-function regulators, including neuroactive steroids,
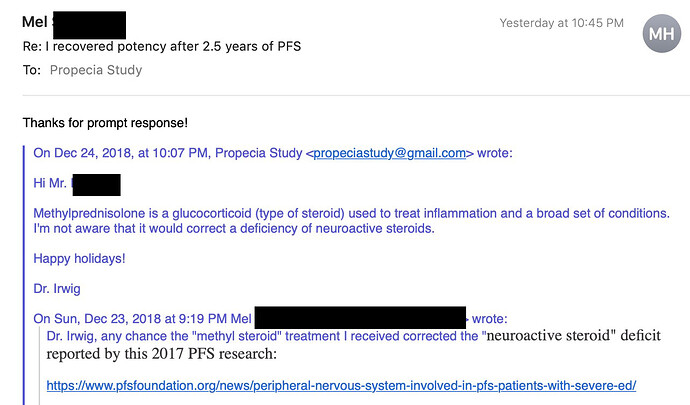
Dr Irwig today wrote me that he believes “methyl steroids” cannot change “neuroactive steroid deficit” in the brain:
It’s encouraging to hear of those who’ve overcome PFS, and while I’ve tried ever over the counter “remedy”, I’m eager to try pharmaceutical solutions to overcome this decade of PFS grief. I’ll do so only under the supervision of a well qualified doctor, and eager to find such a person.
Does such a person exist? I would imagine a doctor who took an interested, collaborative approach would be your best bet in absence of the desired expert.
Unfortunately no such doctor exists, just quacks.
Maybe Dr. Irwig will refer you to some one.
Write him at propeciastudy@gmail.com
But Irwig will probably say “there is no known effective treatment” unfortunately.
I probably just got extremely lucky.