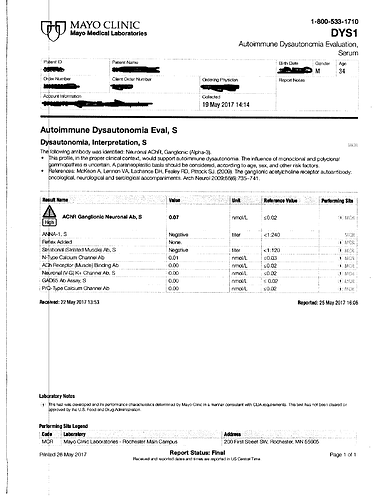
This is one of the more exotic tests I have had, I figured I’d post the results. You also had another Accutane member test positive for this same antibody. Mayo also diagnosed what they called low grade brain inflammation when analyzing his PET scan.
I love the Mayo Hospital. I heard many amazing stories and miracles they’d put on there. If only a group of us could get analyzed there.
So what did they make of this inflammation marker? Did they seem worried about it, or was it just a random test flagged as positive? Did they tell you it definitely meant there was some sort of inflammation or autoimmune reactivity in your head?
Unfortunately its just another piece of the puzzle atm. I had this test ordered locally by my own Dr, using Mayo’s test catalog. It got to the point where I was literally just phoning in blood tests that I wanted to get, and this autonomic dysautonomia panel was one of them.
She had no idea what I had ordered when she got the result back and I actually got scolded a little bit, because she couldnt interpret the results. I went to a local neurologist and he said it was beyond him.
So then I get a referral to a not so far away university, see that neurologist (he was older) and had no idea about this test either, and thats been that so far.
Im only 4 hours away from Mayo in Minnesota, but i’ve been denied before, even with this test result.
I could make a better push with referrals and probably get myself in there if I really wanted to, but ive already had alot of tests, and it will be pretty expensive for me, even with insurance.
I did have a tilt table test for POTS at the University. It was normal.
The other guy that tested positive for this antibody that took Accutane, he did actually take a few trips to Mayo.
I believe they gave him IVIG at Mayo (he said it was expensive) and he continued to do this for awhile.
He didnt say it was a complete cure, and I think he stopped after a few treatments.
This antibody is also on a Mayo panel that looks at gastric dysmotility.
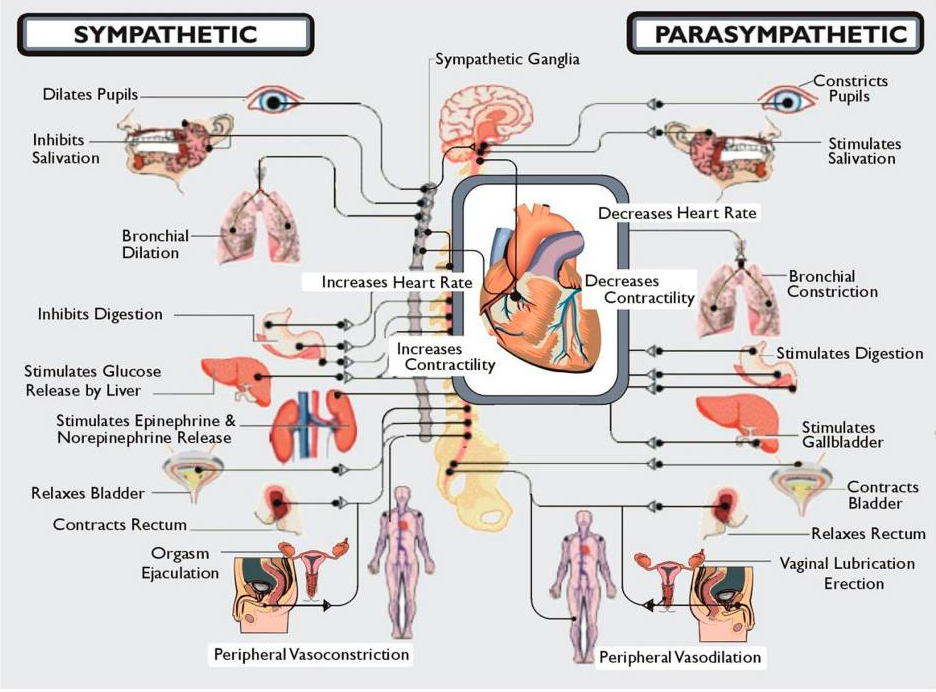
The following image sets out some of the notable features of the ANS.
A good video on this.
Interesting. It could be a random false positive, or just something in the grand scheme of our disease… who knows. I’ll see if Labcorp has it covered in their panel and I’ll get it done if so.
Thanks, man!
Last I knew Labcorp didnt offer this test. Quest did offer this antibody by itself and someone was able to get this test that was on acne.org but tested negative, granted its a different lab though. Mayo I believe only offers this as part of a panel.
Yea this antibody isnt a big focus of mine atm, but as far as a false positive idk.
Of 15 000 patients tested on a service basis, 1% were seropositive
Since incorporating the α3-AChR Ab assay into the standard Mayo Clinic serological evaluation for paraneoplastic autoimmunity in 2005, we have observed that this Ab has broader oncological and neurological associations than originally recognized.
Patients With Low α3-AChR Ab Values
Low values were those between 0.03 and 0.09 nmol/L. The median antibody value in this group of 58 patients (37% of the total) was 0.06 nmol/L. Thirty-one (54%) had either a non–immune-mediated neurological disorder (22 patients) or a nonneurological disorder (9 patients). Twelve (39%) had monoclonal (2 patients) or polyclonal hypergammaglobulinemia (10 patients).
Peripheral neuropathy was the predominant neurological manifestation in 13 patients (22%). Six (10%) had dysautonomia, 3 with pandysautonomia and 3 with limited dysautonomia. Subacute neuropsychiatric presentations were documented in 3 patients, 1 with limbic encephalitis with coexisting ANNA-1 autoantibody and 2 with subacute memory loss and depression. Three patients had myasthenia gravis and were seropositive for muscle AChR–binding Ab (range, 2.56–38.9 nmol/L). Two patients had an inflammatory demyelinating central nervous system disorder, 1 with neuromyelitis optica and 1 with multiple sclerosis.
Yeah I’m not really zoomed in on this at all, although who knows, maybe it is an important finding. Your levels were at .07 nmol/L, and myasthenia gravis had people way higher than that at 2.56 - 38.9. Still an interesting find, though!
Really awesome video. I believe that pfs is dysautonomia related, as its symptoms are closer to autonomic dysfunction than anything else ive seen discussed.
Any idea how an average joe would go about getting this tested?
It would be curious how many people would hit on this antibody out of a pool of all of us post tane,fin,ssri’s.
I would first verify the cpt codes to make sure its covered by insurance. Should be as long as the Dr orders it. A neurologist would be your best bet, but a person might still have to do some strong convincing for any Dr. that is not familiar with these tests. You could say something along the lines of “hey ive had alot of tests and this antibody is showing up in a few people with cases similar to mine”
Also alot of clinics and hospitals are able to send blood work out to Mayo, or have access to their test catalog.
Heres the test.
https://www.mayocliniclabs.com/test-catalog/Overview/92121
Theres also a gi version, (but my gastro dr wasnt at all familiar with this either)
Testing for Autoimmune Disorders
Dysautonomia and Gastrointestinal Dysmotility
Mayo Clinic offers autoantibody evaluations that are tailored to detect all currently recognized IgG markers of autoimmune dysautonomia and gastrointestinal (GI) dysmotility. The ganglionic (alpha 3) acetylcholine receptor (AChR) autoantibody is the most commonly detected marker of autoimmune dysautonomia and is sometimes encountered with isolated GI dysmotility. This is the only autoantibody proven to cause dysautonomia, including GI dysmotility.
Great to know, thank you. My gastric dysmotility is one of my worst symptoms so maybe it would be easy to detect.
I’ve seen you mention it a couple of times now- are you taking meds for your symptoms after these tests?
I’ve been lucky to build on others who have had similar issues and cold showers are absolutely amazing for a host of symptoms, but most importantly the dysmotility, anxiety and sleeping issues.
It must have something to do with the fact that cold showers trigger adrenaline and the divers reflex, maybe it hits a switch in the ans, essentially.
Mine too. So the other guy that I mentioned that was going to Mayo for treatment,
He went every 6 weeks for around a 4 month period. He was getting IVIG treatment at 10k a pop.(his insurance did cover it) He mentioned something about getting his life back and 75 percent cured.
I never talked to him, I believe his last post on acne.org was around 2008.
For me this is a last ditch resort and not very feasible for me atm . Id soon just buy some flonase and swallow it.
On Gi symptoms real quick, dysmotility was also confirmed on a ct scan, they just said to take miralax. they are very basic here locally. I have also been diagnosed with eosinophilic esophagitis multiple times. Again the main treatment is swallowed steroids like flonase. also mild gastritis and I had a colon polyp this past year, so now I get to go back in another 5 years. Awesome.
I am still looking at some things, but I am very careful about any recommendations, we’re still the guinea pig.
I am more and more interested in this theory about cholinergic receptors. Although I don’t think it’s neccesseraly due to antibodies, but maybe just cholinergic muscarinic receptors being silenced… M3 receptors are responsible for functioning of detrusor smooth muscles which pushes the urine out. Muscarinic receptors are also responsible for smooth muscles in heart and other organs, for erections, also for sweating and many many other things we have problems with. And most important thing is that saw palmetto is proven to be big antagonist of muscarinic receptors and inhibits binding of some important things to muscarinic receptors… I definitely can’t push the urine out in a way to make urine flow bigger and faster, and detrusor muscle which is responsible for this from my understanding is controlled by cholinergic muscarinic m3 receptors.
So that’s why we have pelvic floor tension and symptoms? Right?
I believe so yes
Could be also norepinephrine problems
Norepinephrine also controls sweet glands, urine flow (alpha1), lipids (beta3), heart, and so on…