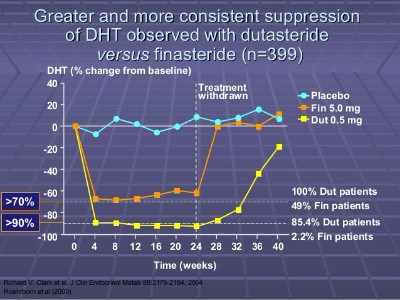
I think a lot of PFS sufferers are dealing with a term coined as withdrawal syndrome after trying to get a better understanding of this condition over the last few months I have decided to look elsewhere, particularly in people who took SSRI’s who try to go off them cold turkey only to be followed with an array of new neurological and physical symptoms many go back on the drug then taper off this is my general understanding of what I have picked up on forums from the people more experienced and who heavily insist in tapering as do doctors so why wouldn’t the same mechanism be applied with finasteride and yes we can’t taper because it has a flat dose response meaning even if we cut it down to 0.2mg it is exactly the same as taking 1mg so we would have to get finasteride right down to 0.01% probably in a liquid solution a good pharmacist could do it. We know for a fact looking at this forum that many users suffer a “crash” this crash is suspected to be hormones coming back into the system at full speed which shut the receptors off as a self protection mechanism. When we take the first pill of finasteride it inhibits 70% of DHT levels for up to 2 weeks after the 2 week mark DHT levels dramatically rise in the body it’s around this time that the majority of people crash because we didn’t taper.
Information I picked up
What causes SSRI withdrawal? Why can some people quit without problems?”
A: The physiological nature of SSRI withdrawal is not well understood, nor is the reason that some have more difficulty with it than others. It is, however, likely that different genetic profiles related to serotonin receptors, etc leads to different levels of severity, different symptom profiles, and ultimately different rates of recovery.
Taking an SSRI causes a variety of neurophysiological changes to occur. Oppositional processes begin almost immediately to offset and adapt to the changes they produce in your brain. Reversing these processes when discontinuing an SSRI is likely a complex, non-linear process that depends on the individual.
|> Q: “Why does this group (and others online) recommend such a slow tapering regimen?”
|===| A: Very slow, non-linear tapering (meaning your reductions will become smaller as you continue to decrease your dose) seems to be the only way to minimize the chances of severe withdrawal symptoms. You will find many accounts of people who have failed two, three, four or more different attempts at tapering until going this route. It can be frustratingly slow, with many people wanting to get the drug out of their system as soon as possible, but we implore you to resist the temptation to do so. This group recommends tapering 5-10% of your dose every 4-6 weeks. (Example: if you are going to try 10%, and your starting dose is 10mg, you would reduce to 9mg, then 8.1mg, then 7.3mg, then 6.6mg, etc.)
Unlike many other drugs, tapering SSRIs can be complex and confusing:
- Symptoms seem to wax and wane over time
- Some reductions are quite easy while others can be far more difficult, with seemingly no pattern to it.
- For many individuals, it can take weeks to stabilize on a new dose.
- Some individuals will experience a delayed withdrawal syndrome that only shows up many week to months after a drop, especially if the taper was quick. I can’t count the number of individuals who quickly stopped an SSRI, felt relatively ok for weeks or months, and then out of nowhere were hit by a severe constellation of withdrawal symptoms.
For more information, and a possible scientific explanation for why slow, non-linear tapering is important, see the following:
http://survivingantidepressants.org/…/1024-why-taper-by-10…/
http://survivingantidepressants.org/…/6036-why-taper-paper…/
|> Q: How do I taper so slowly if they don’t make tablets for each step down?
|===| A: There are a variety of methods to accomplish this.
- If you have the financial means (or good insurance, or live in a country with universal healthcare coverage ) a compounding pharmacy can make (relatively) inexpensive custom dosage capsules for you. This is the easiest and least risky method, as a trained professional is involved.
- You can attempt a switch to the liquid form of the drug you are taking if available. This works for many people, but others have significant problems making the switch from tablets. The liquid form allows easy reductions using an oral syringe.
- If your drug comes in tablet form (not capsules with beads, and not if you are taking an extended release form) you can crush and weigh the powder with a milligram scale. They are relatively inexpensive, and are accurate enough for most people.
- Lastly, if you would like to use a liquid form / suspension of the drug for easy measurement with a syringe but do not have access to a commercial preparation, you can make your own. See this link:
http://survivingantidepressants.org/…/2693-how-to-make-a-l…/
Although suggested by some physicians, alternating doses is not recommended and has given people problems. The exception to this is Prozac, which has a very long half life that minimizes the effects of irregular dosing.
|> Q: What symptoms can I expect tapering or stopping an SSRI?
|===| A: The list of potential withdrawal symptoms is long, and many variations are possible.
Anxiety, nausea, headaches, and “brain zaps” are very common.
Possible cognitive symptoms include memory loss, disorientation, forgetfulness, confusion, and difficulty thinking and communicating clearly.
Possible physical symptoms include blurred vision and eye issues, imbalance, vertigo, intestinal issues, headache, nausea, hot and cold flashes, muscle and joint pain, paresthesia, itchiness/histamine reactions, food sensitivities, restless legs, etc.
Possible emotional symptoms include anxiety, panic, emotional swings, depression, feelings of doom and despair, sensitivity to noise and light, frustration, agitation, heightened flight/flight activity, depersonalization/derealization, stress intolerance, etc.
For more information, see: http://survivingantidepressants.org/index.php…
|> Q: What should I start/avoid during tapering and withdrawal to ease symptoms?
|===| A: Like the withdrawal process itself, everyone seems to react differently, but there are some common patterns. These rules are not hard and fast, but they seem to help many people during this process.
Stimulating substances such as caffeine, nicotine and related commonly exacerbate symptoms and should be avoided. During withdrawal, your sympathetic nervous syndrome can feel like it’s in overdrive, and any further stimulation can cause anxiety, agitation, and overall worsened symptoms.
It cannot be overstated how much one’s diet can affect the course of withdrawal. Sugar and refined grains seem to commonly exacerbate symptoms for many people, as does the ingestion of alcohol.
Many people find regular, moderate exercise to be enormously helpful during withdrawal.
Above all, as you will likely be very sensitive to stress and confrontation, it is best to reduce this as much as is possible in your life.